This week is perinatal mental health week. If you have experienced this please know you are not alone.
Historically, there has been an immense stigma around perinatal mental health issues and people feel like they cannot talk about it.
I had my daughter when I was 22. I had severe physis pubis pain, I couldn’t walk very well, and I had some time with crutches while still trying to work. I have very little family support besides my husband. The constant pain started getting to me & I shared this with the male obstetric registrar, who began doing mental health screening in the most insensitive way. When he got to the question, ‘have you ever thought about hurting yourself or the baby’ I freaked out. I was shocked.
No, of course not.
Was I being judged as a bad mother before I was a mother? As a Torres Strait Islander, I briefly thought, ‘would you take my child from me?’
I had pain. Pain that coloured my whole existence. Every breath, every movement, everything I sensed was through a filter of pain.
I started seeking solutions and saw a physiotherapist and acupuncturist, meditated and reframed my thoughts.
Self care and feeling cared for helped reduce my pain & improved my mood.
Without intervention this could of lead to a perinatal mental illness as I had risk factors.
Around the world right now are parents who feel scared, vulnerable, traumatised and unsure.
Including people who didn’t have the birth they dreamed of.
The childbearing years, especially the first few weeks after childbirth, is the peak period for the onset of depression in women and partners.
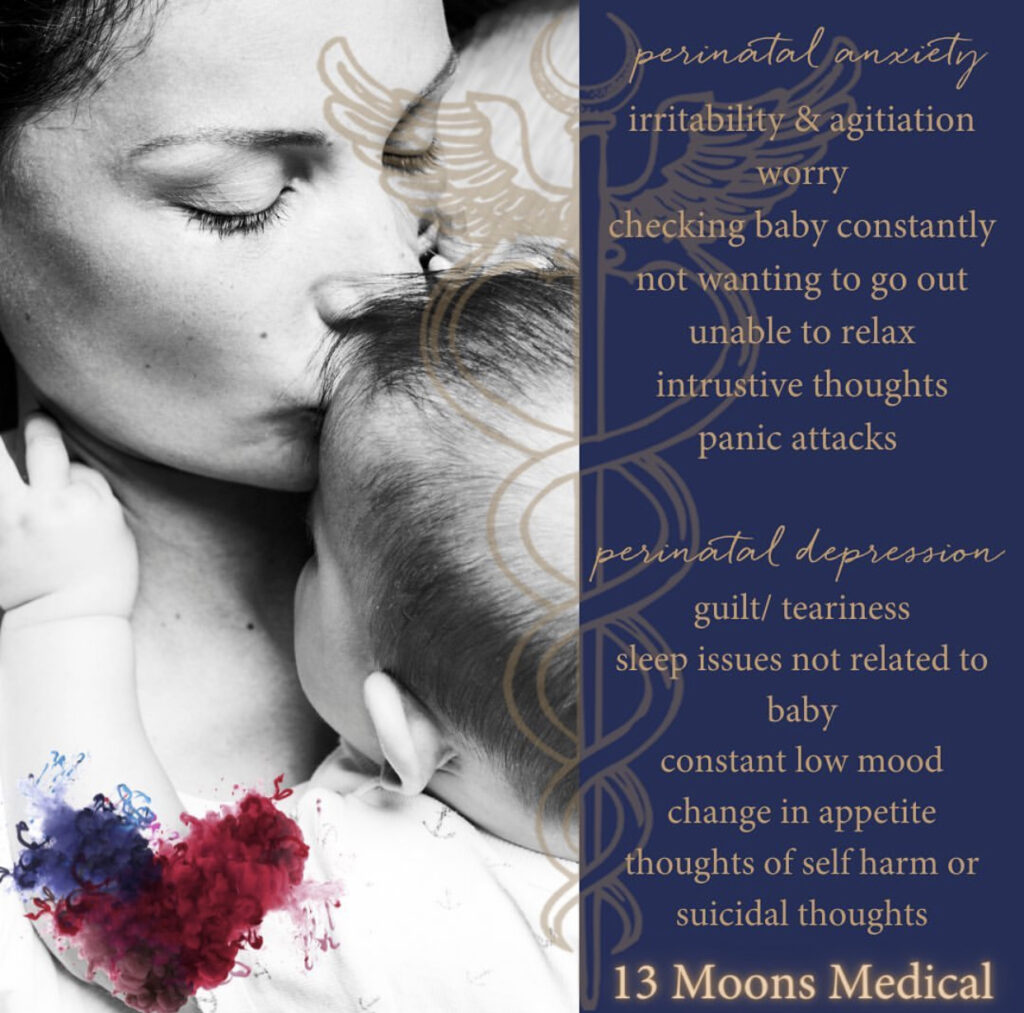
The signs of perinatal anxiety and depression include:
• persistent, generalised worry, often focused on fears for the health of the baby
• mood swings, or feeling constantly sad, low, or crying for no apparent reason
• having little or no interest in all the everyday things that bring joy
• withdrawing from friends and family
• finding it difficult to focus, concentrate or remember
• having thoughts of death or suicide
• changes in appetite: under or overeating
• sleep problems unrelated to the baby’s needs
• loss of confidence and lowered self-esteem
• fear of being alone with baby
• intrusive thoughts of harm to yourself or baby
• increased alcohol or drug use.
Men’s symptoms may be the same as women’s, but some differences exist, including agitation and frustration. They may have out of character outbursts of anger or rage, leading to feelings of shame or guilt. If any of these symptoms are signs, it’s time to get help rather than letting them simmer or keeping them bottled up. ( sane.org)
RISK FACTORS include:
• hormonal changes,
• traumatic pregnancy or birth,
• financial or relationship stress,
• social isolation
• previous reproductive issues such as infertility.
• Trouble breastfeeding, unwell baby
Your history or a family history of mental illness can also increase your risk of developing perinatal mental illness.
Many parents go to great lengths to hide their real feelings because of the stigma associated with mental health issues.
Perinatal mental health causes are multifactorial; if you know someone who has had a baby or worked with women during birth, please be aware of the risk factors, symptoms AND what can be done to help.
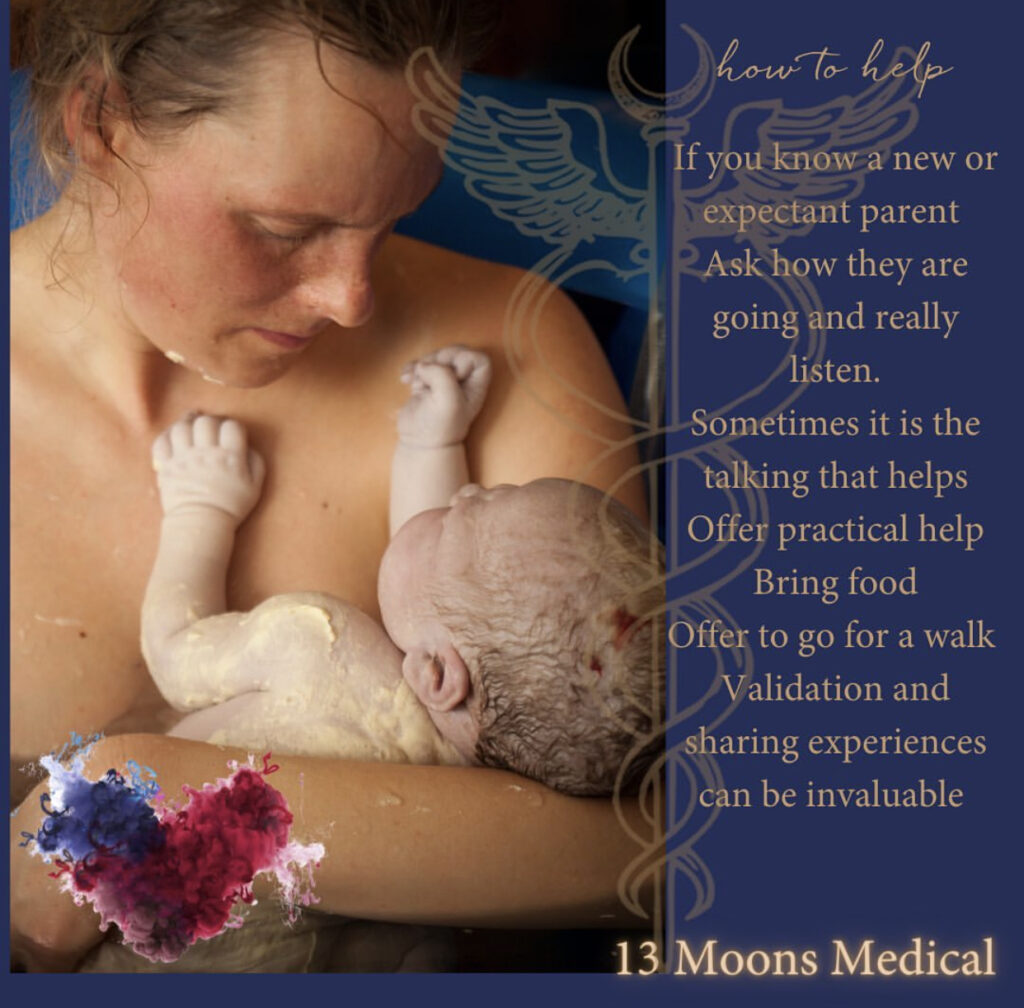
HEALTH AND WELL-BEING INTERVENTIONS
If you suspect that you, your partner, or someone you know may have a perinatal mental illness, support them to seek help from their GP or maternal health nurse. Offer to make the call and go to the appointment. They can also call the PANDA (Perinatal Anxiety & Depression Australia) helpline on 1300 726 306.
Offer to make the call or go to an appointment with them.
Treatment may include:
Therapy with GP, perinatal psychologist or psychiatrist.
Seeing a Midwife, lactation consultant or social worker
Seeing a trauma specialist or relationship counsellor,
Getting Doula support.
Support groups playgroups
And importantly, self-care – yoga, massage, time doing relaxing things
During times of birth, we need our village’s support.
If you need help, please reach out and look after yourselves
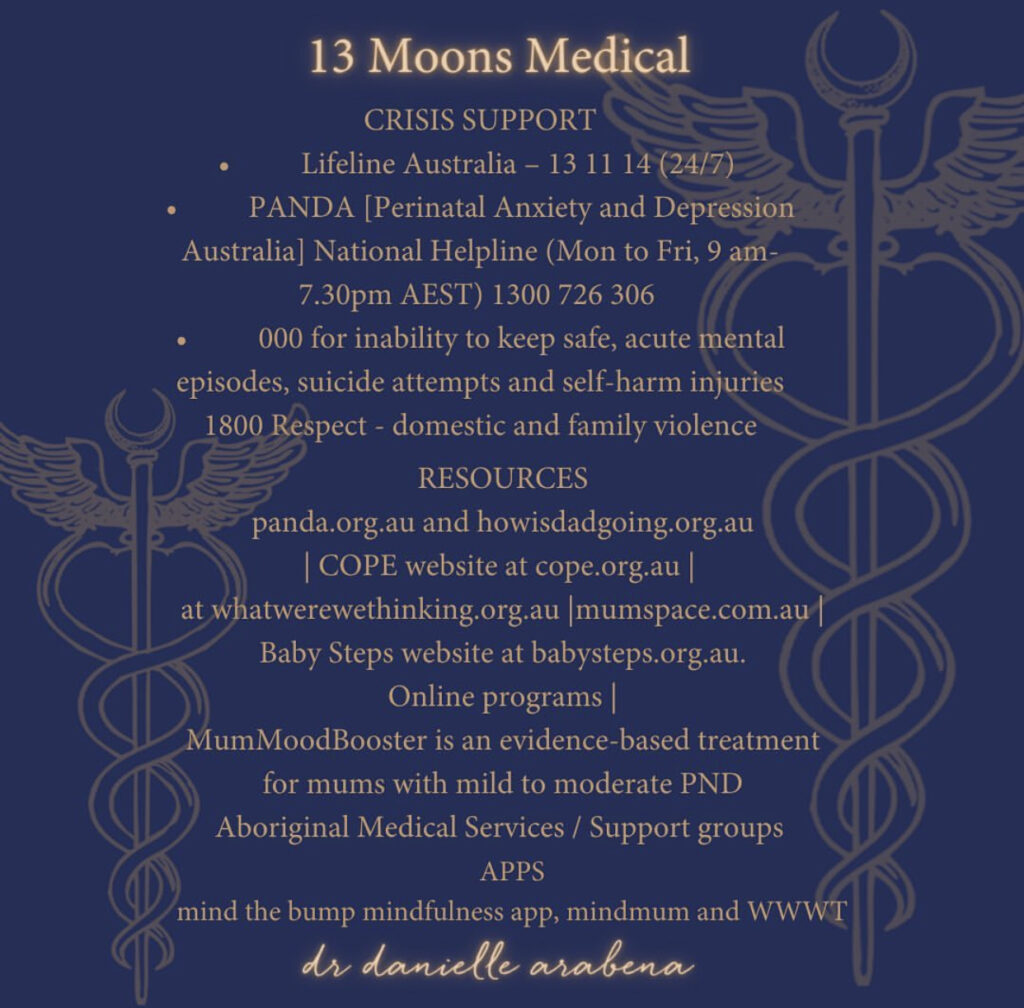
Crisis support
If you need support, call one of the following numbers:
• Lifeline Australia – 13 11 14 (24/7)
• PANDA [Perinatal Anxiety and Depression Australia] National Helpline (Mon to Fri, 9 am- 7.30pm AEST) 1300 726 306
• 000 for inability to keep safe, acute mental episodes, suicide attempts and self-harm injuries